Pathophysiology of Hypertension Made Easy for Kids

Dr P Marazzi / Science Photo Library
Summary box
Hypertension (high blood pressure level) is the leading risk gene associated with decease in the world. It is affected by a wide variety of factors, including increasing historic period, black African or Carribean ethnicity, existence overweight and having a lack of physical activeness. Main hypertension, in which no specific cause is plant, affects 95% of patients.
Hypertension is typically asymptomatic and only detected through opportunisitic screening. Symptoms simply manifest when blood force per unit area reaches very high levels (usually >200 mmHg systolic), and can include headaches, dizziness and nosebleeds.
It is usually diagnosed when a patient's blood force per unit area is repeatedly found to be 140/90 mmHg or higher in a clinical setting and average readings taken using ambulatory blood pressure monitoring or monitoring at domicile are higher than 135/85 mmHg.
In one case hypertension has been diagnosed, further tests should be conducted, including urine testing, blood tests, an center test and a 12-pb electrocardiogram (ECG).
Hypertension is i of the most prevalent cardiovascular take chances factors in the world. Co-ordinate to the World Wellness Organisation, high blood pressure level was the leading risk factor associated with death worldwide in 2004, accounting for 7.5 meg deaths (12.viii% of all deaths). Information technology was the take a chance factor most normally associated with death in heart-income countries (17.two% of all deaths), the second most common in high-income countries afterwards tobacco use (xvi.8% of deaths), and the second most mutual in low-income countries afterwards children existence underweight (7.5% of deaths)[1]
.
In England, 32% of men and 29% of women have, or are being treated for, high blood pressure[2]
. Information from full general do point that much of the hypertension present in the population is currently undetected, with only xiii.eight% of those with the condition identified as hypertensive on GP registers.
| Prevalence of hypertension in the United kingdom of great britain and northern ireland [three] | ||
|---|---|---|
| Number of patients on hypertension register | Detected prevalence (%) | |
| England | 7,698,296 | 13.7% |
| Scotland | 689,650 | 14% |
| Wales | 507,750 | xv.v% |
| Northern Republic of ireland | 501,436 | xiii.1% |
| Total | 9,397,132 | xiii.8% |
| Hypertension past historic period group in the Britain [ 3] | ||
|---|---|---|
| Percentage of population with hypertension | ||
| Historic period range | Men | Women |
| 16–24 years | five | 3 |
| 25–34 years | 6 | 4 |
| 35–44 years | 25 | ten |
| 45–54 years | 37 | 26 |
| 55–64 years | 51 | 47 |
| 65–74 years | 65 | 63 |
| >75 years | 79 | 79 |
Hypertension is one of the most important preventable causes of premature morbidity and bloodshed, and lowering claret pressure reduces the risk of cardiovascular events in people with established hypertension. Each 2 mmHg rising in systolic blood pressure is associated with a vii% increased adventure of death from coronary heart disease and a 10% increased risk of death from stroke[1]
.
Pathophysiology
Claret pressure is expressed in terms of systolic claret pressure (higher reading), which reflects the blood pressure when the heart is contracted (systole), and diastolic blood pressure (lower reading), which reflects the blood pressure during relaxation (diastole). Hypertension can be diagnosed when either systolic pressure level, diastolic pressure, or both are raised.
Claret pressure level is adamant past the cardiac output balanced confronting systemic vascular resistance. The procedure of maintaining claret force per unit area is complex, and involves numerous physiological mechanisms, including arterial baroreceptors, the renin–angiotensin–aldosterone organisation, atrial natriuretic peptide, endothelins, and mineralocorticoid and glucocorticoid steroids. Together, these complex systems manage the caste of vasodilatation or vasoconstriction inside the systemic apportionment, and the retention or excretion of sodium and water, to maintain an adequate circulating blood book.
Dysfunction in whatsoever of these processes tin lead to the development of hypertension. This may be through increased cardiac output, increased systemic vascular resistance, or both.
Claret vessels go less elastic and more than rigid as patients age, which reduces vasodilatation and increases systemic vascular resistance, leading to a college systolic blood pressure (often with a normal diastolic pressure). In contrast, hypertension in younger patients tends to exist associated with increased cardiac output, which tin be acquired by environmental or genetic factors.
Take a chance factors for developing hypertension include:
- increasing age (50% of the population aged over 60 years have hypertension)
- ethnicity — hypertension is more prevalent in patients of Black African or Caribbean descent
- being overweight or obese
- physical inactivity
- excess common salt consumption
- backlog alcohol intake
- stress
- other medical conditions (e.g. diabetes, chronic kidney disease, slumber apnoea).
No specific crusade of hypertension is institute for almost (>95%) patients with high blood pressure level, and this is frequently referred to every bit chief or essential hypertension. Secondary causes are identified in the remaining five% of cases. The list of possible causes is all-encompassing, and includes:
- medicines (east.g. non-steroidal anti-inflammatory drugs, oral contraceptives, corticosteroids, sympathomimetics)
- renovascular disease
- pheochromocytoma
- primary hyperaldosteronism (e.g. Conn's syndrome)
- coarctation (narrowing) of the aorta
- Cushing's syndrome.
Patients with suspected secondary hypertension should be referred to a specialist squad.
Clinical features
Hypertension is not a illness in its own right, merely if left untreated information technology is a hazard factor for astute events (such as myocardial infarction and stroke) and for the development of organ impairment.
Chronically raised claret force per unit area can lead to several conditions related to pressure overload:
- left ventricular hypertrophy, which is the result of chronic pressure overload in the myocardium, resulting in thickening of the muscle; this slows ventricular relaxation and delays filling during diastole, reducing the efficiency of the centre as a pump.
- exacerbation of the development of coronary heart disease, which results in myocardial ischaemia or infarction
- heart failure, as the ability of the heart to meet the demands of the torso falls
- thromboembolic or haemorrhagic strokes or transient ischaemic attacks (TIAs)
- chronic kidney disease with proteinuria or albuminuria, every bit renal perfusion is afflicted
- retinopathy and haemorrhages of the fundus (the inner surface of the eye).
Hypertension is asymptomatic in most cases, only beingness detected through opportunistic screening. Symptoms only manifest when the blood pressure reaches very high levels (normally >200 mmHg systolic), and can include headaches, dizziness and nosebleeds. Many patients tolerate high claret pressures (even in excess of 180 mmHg systolic) for significant periods without symptoms or any adverse effects, although these patients are at significant take a chance of experiencing an acute effect or damage to organs including the encephalon, optics, heart and kidneys.
Malignant, old referred to every bit accelerated, hypertension is very high claret pressure that occurs suddenly without alarm, and can involve systolic blood pressures in backlog of 200 mmHg and diastolic claret pressure level above 130 mmHg. Malignant hypertension is a medical emergency and requires urgent treatment to limit the acute damage to the brain, eyes, blood vessels, heart and kidneys.
Key signs of accelerated hypertension include blood pressure of >180/110 mmHg associated with signs of papilloedema, retinal haemorrhage, or suspected phaeochromocytoma (which include labile or postural hypotension, headache, palpitations, pallor and diaphoresis). Patients with suspected accelerated hypertension should be referred urgently for review by a specialist on the same twenty-four hours.
Diagnosis
Traditionally, hypertension has been identified by checking a patient's blood pressure in a dispensary repeatedly over a menses of 2–3 months. Hypertension was confirmed if the systolic claret pressure was persistently greater than 140 mmHg, or the diastolic claret pressure was persistently greater than 90 mmHg.
This method of diagnosis has significant limitations because the claret pressure level measured in the clinic setting may non reflect the claret pressure in day-to-day life. In detail, there are concerns that claret pressure may exist artificially raised in the dispensary setting in some patients, often referred to every bit 'white glaze hypertension', which could result in people receiving unnecessary drug handling[4]
.
However, in Baronial 2011 the National Constitute for Health and Care Excellence (Overnice) published guidance that brought significant changes to diagnosis in England[5]
. This included the recommendation that hypertension should be diagnosed using ambulatory claret pressure monitoring (ABPM) or dwelling house blood pressure level monitoring (HBPM)[5]
. I of these methods should be used to confirm the diagnosis of hypertension following the recording of a high blood pressure reading in the dispensary setting.
Ambulatory blood pressure monitoring is a non-invasive method of obtaining blood pressure readings over a 24-hour menses while the patient goes about their normal activities of daily life. Blood pressure measurements are taken every one-half hr during the solar day and every 60 minutes at dark. A patient is diagnosed with hypertension if the average of the daytime blood pressure level readings is greater than 135/85 mmHg. Although the night-time pressures are not used, they provide boosted information, including whether the patient is a 'night-time dipper' (the claret force per unit area goes down overnight while comatose); if this does not occur, the patient is at a higher chance of cardiovascular disease.
The success of ambulatory blood force per unit area monitoring is reliant on the machine beingness correctly fitted, and a proportion of readings tin fail (for example, if the tubing becomes kinked at the time of cuff aggrandizement). Information technology is therefore important to ensure that the daytime average claret pressure level used to diagnose hypertension is based at least 14 successful daytime claret pressure readings. ABPM is the method of pick for diagnosing hypertension in the NICE guidance, equally it is the most cost-effective strategy when compared with clinic or HPBM, and there is substantial testify that it is better than blood force per unit area measurements in the dispensary for predicting future cardiovascular events and target organ damage[4]
.
Home blood pressure monitoring involves the patient taking blood force per unit area readings in the morning and evening for seven days at home and recording the results. Each reading involves ii consecutive measurements taken at least one infinitesimal apart while the patient is seated.
The first 24-hour interval's results are discarded, and an average of the results of all other readings is calculated. A patient is diagnosed with hypertension if this average is at least 135/85 mmHg[v]
.
It is essential that the patient is supplied with a validated and calibrated blood pressure machine to ensure the accuracy of the readings taken. A list of validated blood pressure machines can exist found on the British Hypertension Gild website (http://www.bhsoc.org/bp-monitors/bp-monitors).
Staging
Staging is used to guide management options and the urgency with which the raised blood force per unit area should be addressed. For example, in severe hypertension, the diagnosis should be made using claret pressure level readings from the clinic, and handling should exist started without delay (see 'Traffic-light guide to claret pressure level management').
Traffic-low-cal guide to blood pressure level (BP) management
How to assess patients and the actions you would demand to take.
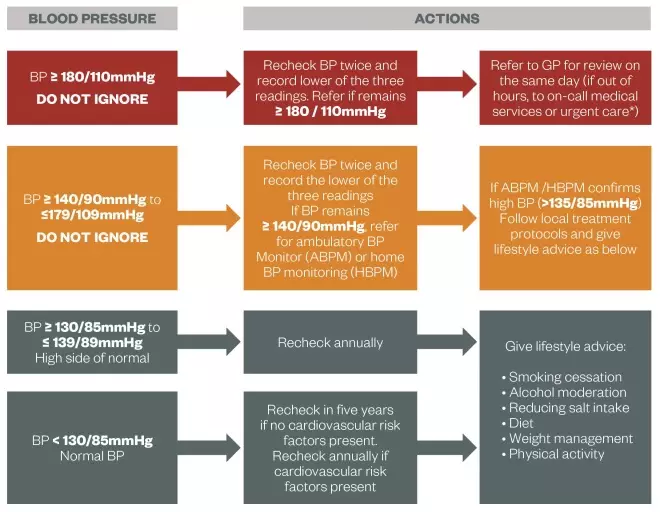
Source: South East London Expanse Prescribing Committee and Southward West London Medicines Commissioning Group
*Particularly if accelerated hypertension (blood pressure usually college than 180/110 mmHg with signs of papilloedema and/or retinal haemorrhage) or suspected phaeochromocytoma (labile or postural hypotension, headache, palpitations, pallor and diaphoresis).
High-adventure patients
Once diagnosed, all patients with hypertension should have a series of further tests and investigations:
- urine testing for the presence of protein by checking the albumin:creatinine ratio (ACR) and testing for haematuria using a reagent strip
- blood tests to measure plasma glucose, electrolytes, creatinine, estimated glomerular filtration rate (eGFR), serum total cholesterol and loftier-density lipoprotein (HDL) cholesterol
- eye test to check for hypertensive retinopathy
- a 12-lead electrocardiogram (ECG) to check for signs of left ventricular hypertrophy or ischaemia.
People younger than twoscore years of agewith hypertension should also be considered for specialist referral to found if at that place is any underlying causes of hypertension and to identify whatsoever early target organ damage.
A full cardiovascular risk assessment should be undertaken for all patients (except in the presence of pre-existing cardiovascular disease; in England and Wales, NICE recommends the using the QRisk2 calculator (www.qrisk.org), although others are available. This takes into account the patient's age, gender, ethnicity, claret pressure and total cholesterol:HDL ratio as a minimum to calculate the percentage chance of developing cardiovascular disease over the next ten years. Patients with a cardiovascular-disease hazard of ≥ 20% require more intensive handling for their hypertension.
Other patients with a higher risk of hereafter cardiovascular events also crave more intensive treatment (come across 'Hypertension: management'). This includes patients with established cardiovascular disease (prior coronary heart affliction, stroke or transient ischaemic attack, or peripheral arterial disease), diabetes and chronic kidney disease.
Helen Williams is a consultant pharmacist for cardiovascular affliction at Southwark Clinical Commissioning Group.
References
[1] Globe Health Organization. Global Health Risks: Mortality and Brunt of Illness Attributable to Selected Major Risks. Geneva: WHO 2009.
[2] Joint Health Surveys Unit.Health Survey for England 2010. Leeds: The Information Centre, 2011.
[3] British Center Foundation. Coronary Heart Disease Statistics. London: British Centre Foundation, 2012
[iv] Lovibond K, Jowett S, Barton Pet al. Price-effectiveness of options for the diagnosis of high blood pressure in master care: a modelling study.Lancet 2011, doi: ten.1016/S0140-6736(11)61184-vii.
[five] National Plant for Health and Care Excellence. Hypertension: Clinical Management of Chief Hypertension in Adults. London: NICE, 2011.
Final updated
carpenterlielf1997.blogspot.com
Source: https://pharmaceutical-journal.com/article/ld/hypertension-pathophysiology-and-diagnosis
Enregistrer un commentaire for "Pathophysiology of Hypertension Made Easy for Kids"